By Dr Gab General Practitioner Specialising in women’s health, with a particular focus on menopause care
Osteoporosis is often called a “silent disease” — most people don’t know they have it until they suffer a fracture. Yet it affects millions of Australians and significantly impacts quality of life, especially in older women.
What is Osteoporosis?
Osteoporosis is a chronic condition where bones become weak, brittle, and more prone to fractures — even from minor falls or, in some cases, no obvious trauma at all. It's different from osteopenia, which is a state of lower-than-normal bone density that hasn’t yet progressed to osteoporosis but still increases fracture risk.
Fast Facts:
On average, women lose 5% of their bone density in the first five years after menopause, with bone loss typically beginning in the years leading up to menopause.
In Australia, 1.2 million people are living with osteoporosis, and 6.3 million have low bone density (osteopenia).
The incidence of osteoporosis is more common in women compared to men because of the hormonal differences1 in 2 postmenopausal women will suffer from a fragility fracture.
Among women who experience a hip fracture due to osteoporosis; Less than 50% return to their pre-fall function; 25% will die within the first year after the fracture.
Why Are Women at Higher Risk?
Estrogen plays a vital role in maintaining bone strength. After menopause, estrogen levels drop sharply, accelerating bone loss. Women who go through early or premature menopause are at even higher risk.
Other Risk Factors Include:
- Gastrointestinal absorption issues (e.g. coeliac disease)
- Long-term use of steroids
- Smoking
- Eating disorders
- Autoimmune conditions
- Thyroid disease
How to Protect Your Bones
Maintaining strong bones throughout life is essential — and prevention is far easier than treatment after a fracture has occurred. Here are some key strategies:
- Estrogen Matters: For women going through menopause, hormone therapy may be recommended to protect against bone loss, especially if started early in the menopausal transition.
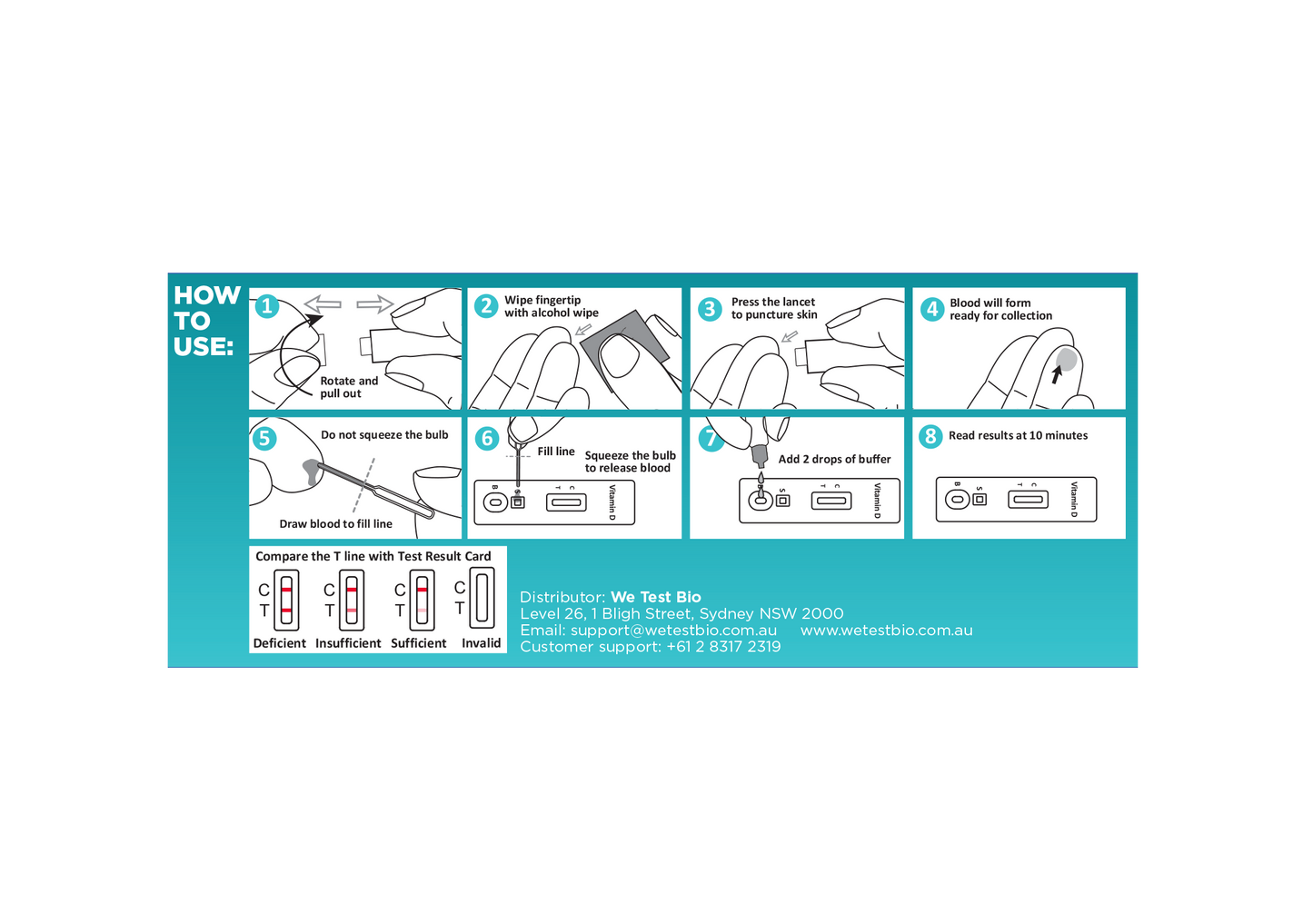
- Calcium and Vitamin D Calcium: Aim to get calcium through diet (dairy, leafy greens, almonds, tofu, and fortified foods).Vitamin D: Your body needs sunlight to produce vitamin D, which helps absorb calcium. If your levels are low, supplementation may be necessary.
- Weight-Bearing Exercise Exercise tells your bones they need to stay strong. Weight-bearing and resistance exercises stimulate bone turnover and help maintain density. This includes: Lifting or pulling heavy objects Jumping, skipping, or impact aerobics Resistance training like squats, lunges, or using resistance bandsWhile walking doesn’t offer much in terms of bone health – it’s a great place to start and it offers benefits in other areas including maintaining cardiovascular fitness as well as promoting health muscle mass and balance.
- Regular Screening If you're over 50 and have risk factors — or if you've had a fracture from a minor fall — talk to your doctor about getting a bone density scan (DEXA scan).In Australia, Medicare subsidises a DEXA scan for anyone aged 70 and over, even without specific risk factors. If you're under 70 and don’t meet the criteria for a rebate, you can still have the scan done privately for a fee. It’s a simple, painless test that can provide critical information about your fracture risk.
OK – But what about Sarcopenia
Sarcopenia is the age-related loss of muscle mass and strength — and like osteoporosis, it accelerates after menopause. While bone health often gets more attention, muscle loss is just as important when it comes to maintaining mobility and preventing frailty.
Key Points:
Women lose approximately 5–10% of muscle mass per decade after menopause.
Muscle loss often becomes evident when strength and function begin to decline — typically before noticeable changes in size.
Postmenopausal women experience a rapid drop in muscle mass and strength, making them more vulnerable to falls, frailty, and reduced independence.
What Can Help?
Interventions that can help slow or reverse sarcopenia include:
Nutritional strategies:
- Adequate protein intake
- Vitamin D supplementation if deficient
- Emerging evidence supports the use of creatine to improve muscle strength and function
Exercise:
- Especially resistance training, which directly stimulates muscle growth and improves strength
Estrogen:
- Estrogen plays an important role in maintaining muscle health. Its decline in menopause contributes to the drop in muscle mass and function.
- Menopausal Hormone Therapy (MHT) may help preserve or improve muscle mass — especially when combined with regular resistance training.
Takeaway:
Osteoporosis and sarcopenia are two major, often silent changes that affect women’s health after menopause. By staying informed and proactive — with nutrition, movement, screening, and possibly hormone support — it’s possible to protect both bone and muscle health, maintain strength, and reduce the risk of fractures and frailty as you age.